Smart Therapies: How AI is Making Treatment More Effective
Early detection of diseases is crucial for successful treatment. The earlier a disease is identified, the greater the chances of successful treatment and improved patient outcomes. AI's ability to process large datasets and identify subtle patterns allows for earlier detection of various diseases, even before symptoms appear.
Early detection translates to better treatment options and a higher probability of positive outcomes. This is especially important for diseases like cancer, where early intervention can drastically improve survival rates. AI-driven diagnostics can help identify precancerous changes or anomalies long before they manifest as noticeable symptoms, enabling prompt intervention.
Challenges and Considerations
While AI offers tremendous potential in AI-driven diagnostics, there are important challenges and considerations to address. One key concern is the need for high-quality, reliable data to train AI algorithms. Inaccurate or incomplete data can lead to inaccurate diagnostic results. Data privacy and security are also crucial considerations, particularly as AI systems process sensitive patient information.
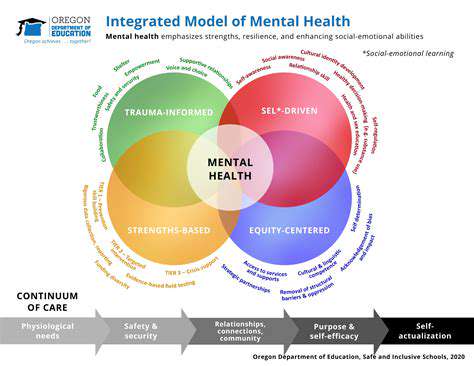
Ensuring the ethical use of AI in healthcare is paramount. Bias in the training data can lead to unfair or inaccurate diagnoses for certain patient populations. Transparency and explainability of AI decision-making processes are also essential for building trust and ensuring responsible application.
The Future of AI in Diagnostics
The future of AI in diagnostics holds immense promise. Ongoing research and development are focused on improving the accuracy, reliability, and accessibility of AI-driven diagnostic tools. This will likely involve the development of more sophisticated algorithms, the creation of larger, more diverse datasets, and the integration of AI systems with existing healthcare infrastructure.
Advancements in AI technology are poised to revolutionize healthcare by making diagnostics more efficient, accurate, and accessible. This will not only improve patient care but also contribute to a more sustainable and equitable healthcare system globally.
The Future of Smart Therapies: Ethical Considerations and Accessibility
Data Privacy and Security in Smart Therapies
Protecting patient data is paramount in the development and implementation of smart therapies. Robust encryption methods, secure data storage protocols, and strict access controls are essential to prevent unauthorized access and breaches. Furthermore, clear and transparent data privacy policies, readily understandable by patients, must be implemented and rigorously adhered to. This includes mechanisms for patients to review, correct, and delete their data, as well as provisions for data anonymization and de-identification when appropriate.
The increasing reliance on algorithms and AI in smart therapies raises concerns about algorithmic bias. Careful consideration must be given to ensuring that these systems are trained on diverse and representative datasets to prevent the perpetuation of existing societal biases. Regular audits and evaluations of these systems are necessary to identify and mitigate potential biases, ultimately ensuring equitable access and outcomes for all patients.
Accessibility and Equity in Smart Therapy Delivery
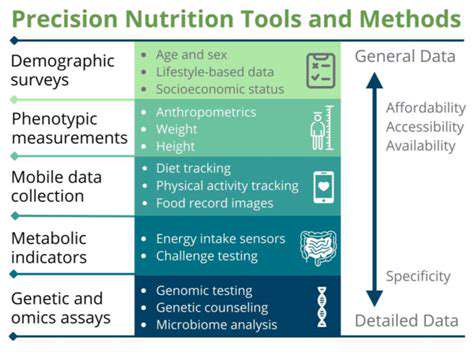
Ensuring equitable access to smart therapies is critical. Cost considerations are paramount, and affordability must be a key design principle. Innovative financing models, such as subsidies or payment plans, should be explored to make these technologies accessible to a wider range of individuals, irrespective of socioeconomic status. This includes considering the digital divide, ensuring reliable internet access, and providing training and support for individuals who may lack the necessary digital literacy skills.
Geographical disparities in access to healthcare services must be addressed. Smart therapies should be designed and implemented to facilitate remote delivery, enabling access for individuals in underserved communities who may face significant barriers to traditional healthcare.
The Role of Healthcare Professionals in Smart Therapies
Healthcare professionals play a crucial role in guiding patients through the implementation and use of smart therapies. Training programs for healthcare providers are essential to equip them with the knowledge and skills necessary to effectively integrate these technologies into their practice. This includes understanding the capabilities, limitations, and potential risks associated with specific smart therapies, as well as how to effectively communicate this information to patients.
Collaboration between healthcare professionals and technology developers is vital to ensure that smart therapies are aligned with established clinical guidelines and best practices. This collaborative approach will facilitate the development of safe, effective, and ethically sound smart therapies.
Regulatory Frameworks and Standards for Smart Therapies
Clear regulatory frameworks are needed to govern the development, testing, and deployment of smart therapies. These frameworks should address issues such as data privacy, safety, efficacy, and liability. Collaboration between regulatory bodies, technology developers, and healthcare professionals is essential to establish comprehensive and adaptable standards that evolve with the advancements in technology.
Establishing clear guidelines for the use of AI and algorithms in healthcare is a crucial aspect of responsible innovation. This includes defining the roles and responsibilities of different stakeholders, such as developers, clinicians, and patients, in ensuring accountability and transparency.
Ethical Considerations Regarding Patient Autonomy and Consent
Patient autonomy and informed consent are paramount in the development and implementation of smart therapies. Patients must have the right to understand how their data is being used, what the potential benefits and risks are, and the ability to make informed decisions about their participation. This includes ensuring that patients have adequate understanding of the technology's capabilities and limitations, and the potential consequences of using or not using the therapy.
Transparent communication and clear consent mechanisms are vital for building trust and ensuring that patients feel empowered to make choices that align with their values and preferences.
Impact on Healthcare Workforce and Job Roles
The integration of smart therapies will undoubtedly impact the healthcare workforce. New roles and responsibilities may emerge, requiring adaptation and retraining of current professionals. Healthcare providers will need to adapt to new tasks, such as monitoring patient data, interpreting algorithm outputs, and providing support to patients using smart therapies. New training programs and educational initiatives are needed to prepare the healthcare workforce for these evolving roles.
The potential displacement of certain traditional healthcare roles must be carefully considered. Re-skilling and upskilling initiatives will be crucial to ensure a smooth transition and maximize the benefits of smart therapies while minimizing potential negative impacts on the workforce.
Long-Term Implications and Societal Impact
The long-term implications of smart therapies extend beyond individual patient care. These technologies have the potential to revolutionize healthcare delivery, potentially reducing costs, improving outcomes, and expanding access to care on a global scale. However, careful consideration must be given to the societal impact of these innovations, including potential disruptions to existing healthcare systems and the need for robust support structures for vulnerable populations.
Addressing the ethical and social implications of smart therapies proactively will help ensure that these technologies are used responsibly and equitably, fostering a healthier and more sustainable future for all.