Personalized Approaches to Eating Disorder Recovery
Understanding the Whole-Person Evaluation
The Essence of Comprehensive Patient Evaluation
Modern healthcare demands more than symptom-focused examinations. A thorough patient evaluation explores the complex interplay between biological, psychological, and social factors influencing health. This multidimensional perspective examines not just immediate concerns but also lifestyle patterns, environmental influences, and personal history. Only by understanding these connections can clinicians develop interventions that target fundamental causes rather than superficial manifestations.
Honoring Individual Differences
Each patient brings a unique life story to the clinical encounter. Effective healthcare professionals recognize how cultural traditions, economic circumstances, and personal beliefs shape health perceptions. By adapting assessment methods to these individual characteristics, clinicians create more meaningful and effective care strategies. This personalized approach fosters stronger therapeutic relationships and better health outcomes.
Diverse Evaluation Methods
Comprehensive assessment requires multiple investigative tools working in concert. Clinical interviews, standardized assessments, physical exams, and functional evaluations together provide a complete clinical picture. This methodological diversity prevents overreliance on any single data source while improving diagnostic accuracy. When combined thoughtfully, these tools reveal patterns that might otherwise remain hidden.
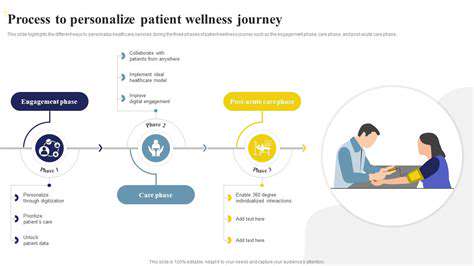
Creating Personalized Care Strategies
Partnership in Treatment Development
Effective care plans emerge from true collaboration between patients and providers. When patients actively contribute to planning, they demonstrate greater commitment to following recommendations. This participatory approach respects patient autonomy while ensuring interventions align with personal values and practical realities. The resulting sense of ownership significantly improves adherence and outcomes.
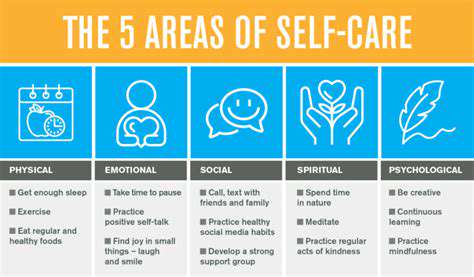
Lifestyle Integration
Daily habits profoundly influence health trajectories. Comprehensive care plans intentionally address nutrition, physical activity, sleep quality, social connections, and stress management. These lifestyle elements often determine the success or failure of medical interventions. For instance, combining medication with customized dietary adjustments typically yields better results than pharmacology alone.
Continuous Plan Refinement
Static treatment protocols rarely serve patients well over time. Regular progress evaluations allow for necessary adjustments as circumstances change. This dynamic approach ensures interventions remain relevant as patients evolve through their healing journey. The flexibility to modify strategies based on real-world feedback distinguishes exceptional healthcare.
Nutrition's Role in Medical Care

Interprofessional Collaboration
Nutritional guidance integrated with medical treatment produces superior health outcomes. When physicians and nutrition specialists coordinate care, patients receive more comprehensive support. This team approach recognizes food as fundamental medicine, particularly for chronic conditions. Shared patient records and regular case discussions ensure all providers work toward common goals.
Customized Dietary Planning
Effective nutrition interventions require personalization beyond standard guidelines. Individualized plans consider medical conditions, food preferences, cultural traditions, and practical constraints. This tailored approach moves beyond calorie counting to address specific nutrient needs and metabolic considerations. Practical implementation strategies increase the likelihood of lasting dietary changes.
Condition-Specific Nutrition
Therapeutic diets play critical roles in managing numerous health conditions. For diabetes patients, carbohydrate management stabilizes blood sugar levels. Cardiovascular patients benefit from lipid-modifying eating patterns. Evidence-based nutritional strategies complement medical treatments across diverse specialties, from oncology to nephrology to gastroenterology.
Lifestyle Foundations for Health
Movement as Medicine
Regular physical activity remains among the most powerful health interventions. Consistent moderate exercise provides cardiovascular, metabolic, and mental health benefits that rival pharmaceuticals. Sustainable routines built around enjoyable activities prove more effective than intense, short-lived fitness regimens. Simple strategies like walking meetings or active commuting can dramatically improve wellbeing.
Mindful Eating Practices
Nutritional quality significantly impacts disease risk and energy levels. Emphasizing whole foods while minimizing processed products creates a foundation for vitality. Gradual dietary improvements, supported by professional guidance, lead to more lasting change than extreme restrictions. Understanding food's medicinal properties empowers patients to make informed daily choices.
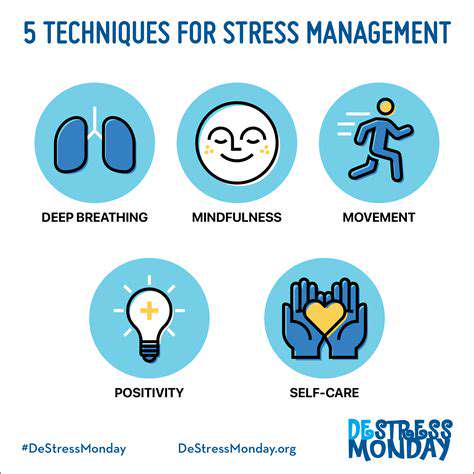
Stress Resilience Techniques
Chronic stress undermines both physical and mental health. Practical stress-reduction techniques like breathwork and mindfulness meditation help restore physiological balance. These evidence-based practices enhance emotional regulation while reducing inflammation and other stress-related pathologies. Regular practice builds resilience against life's inevitable challenges.
Read more about Personalized Approaches to Eating Disorder Recovery
Hot Recommendations
- AI Driven Personalized Sleep Training for Chronic Insomnia
- AI Driven Personalization for Sustainable Stress Management
- Your Personalized Guide to Overcoming Limiting Beliefs
- Understanding Gender Dysphoria and Mental Health Support
- The Power of Advocacy: Mental Health Initiatives Reshaping Society
- Building a Personalized Self Compassion Practice for Self Worth
- The Ethics of AI in Mental Wellness: What You Need to Know
- AI Driven Insights into Your Unique Stress Triggers for Personalized Management
- Beyond Awareness: Actionable Mental Health Initiatives for Lasting Impact
- Creating a Personalized Sleep Hygiene Plan for Shift Workers