Government & Policy: Driving Mental Health Initiatives for Societal Change
Implementing Policy Changes for Equitable Access to Care
Understanding the Need for Change
Implementing policy changes for equitable access to care is crucial for a just and thriving society. Unequal access to healthcare services often exacerbates existing societal disparities, leading to poorer health outcomes for marginalized communities. Analyzing these disparities and identifying the root causes—including socioeconomic factors, geographic limitations, and systemic biases—is essential for developing effective and targeted interventions. This process necessitates a deep understanding of the specific challenges faced by each community, including those related to language barriers, cultural norms, and socioeconomic limitations.
A fundamental aspect of this process is acknowledging the historical and ongoing systemic factors that have contributed to these disparities. Understanding these factors provides a framework for developing policies that address the root causes rather than simply treating the symptoms.
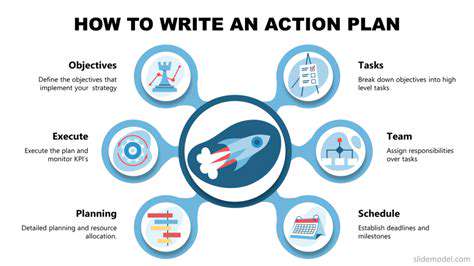
Developing Comprehensive Policy Solutions
Developing effective policy solutions requires a multi-faceted approach, encompassing a range of strategies. This involves considering financial incentives and subsidies for preventative care, expanding access to affordable healthcare providers in underserved areas, and implementing policies that promote health literacy and awareness within communities. Furthermore, addressing the underlying socioeconomic factors contributing to health disparities, such as poverty and lack of education, is crucial for creating lasting solutions.
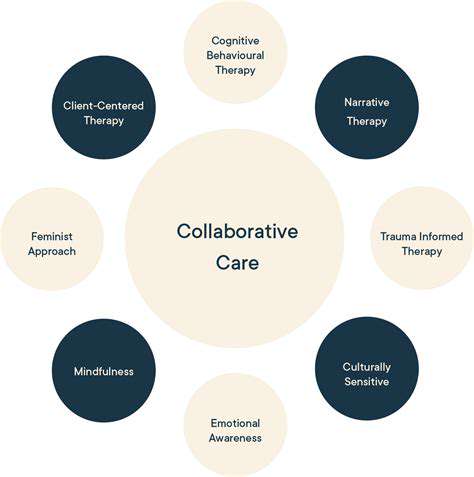
These solutions should also consider the importance of culturally competent care. Policies need to acknowledge and address the unique needs of diverse communities, ensuring that healthcare services are sensitive to cultural nuances and language barriers. This often involves training healthcare providers to better understand and respond to the needs of diverse populations.
Implementing and Evaluating Policy Effectiveness
Implementing policy changes is not a one-time event; it requires ongoing monitoring and evaluation to ensure that the intended goals are being met. This involves rigorous data collection, analysis, and reporting on the impact of the implemented policies on health outcomes for various populations. Tracking changes in access, utilization of services, and overall health indicators is vital for identifying areas needing adjustment and refinement. A critical component of this process involves engaging with stakeholders, including community leaders, healthcare providers, and patients, to gather feedback and ensure that the policies are relevant and effective.
Regular evaluation should assess not only the quantitative impact but also the qualitative aspects, such as patient satisfaction and the perceived equity of the care delivery system. This holistic approach ensures that policies are not only achieving their intended goals but also fostering a sense of community and trust in the healthcare system.
Ensuring Sustainability and Long-Term Impact
Ensuring long-term success hinges on the sustainability of implemented policies. This requires building support within the political and bureaucratic structures to maintain funding and resources for ongoing programs. Furthermore, fostering partnerships with community organizations and stakeholders is essential for ensuring that the policies remain relevant and adaptable to evolving community needs. Continuous engagement with stakeholders is paramount for maintaining buy-in and promoting the long-term success of these initiatives.
Long-term impact also requires a commitment to ongoing training and professional development for healthcare providers. This allows them to adapt to emerging challenges and continue to deliver culturally competent and equitable care. This proactive approach ensures that policy changes are not simply temporary fixes but are woven into the fabric of the healthcare system for lasting improvement.

Read more about Government & Policy: Driving Mental Health Initiatives for Societal Change
Hot Recommendations
- AI Driven Personalized Sleep Training for Chronic Insomnia
- AI Driven Personalization for Sustainable Stress Management
- Your Personalized Guide to Overcoming Limiting Beliefs
- Understanding Gender Dysphoria and Mental Health Support
- The Power of Advocacy: Mental Health Initiatives Reshaping Society
- Building a Personalized Self Compassion Practice for Self Worth
- The Ethics of AI in Mental Wellness: What You Need to Know
- AI Driven Insights into Your Unique Stress Triggers for Personalized Management
- Beyond Awareness: Actionable Mental Health Initiatives for Lasting Impact
- Creating a Personalized Sleep Hygiene Plan for Shift Workers