AI in Substance Abuse Treatment: Personalized Recovery Paths

Predictive Analytics for Early Intervention
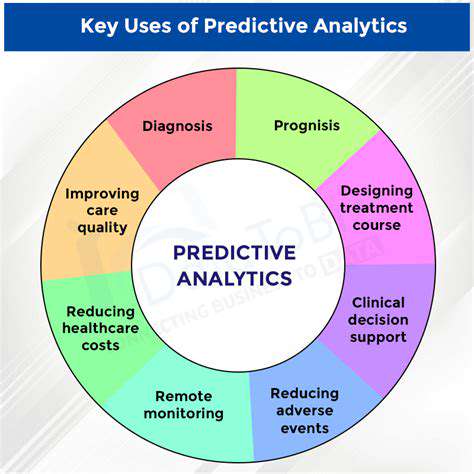
Predictive Modeling for Early Intervention
Recent advances in data analysis now enable professionals to spot potential developmental delays or behavioral concerns much earlier than before. By examining a mix of medical records, family histories, and environmental influences, these analytical tools can detect subtle patterns indicating a higher probability of needing support. This forward-looking strategy creates opportunities for timely assistance, potentially reducing the lasting effects of these challenges.
Research consistently shows that support programs yield better results when started before significant delays become apparent. This preventative method lets specialists tackle emerging needs and promote healthy growth patterns. Modern analytical techniques serve as invaluable allies in this process, pinpointing children who could gain from early support, sometimes even before any clear signs emerge.
Information Sources and Key Factors
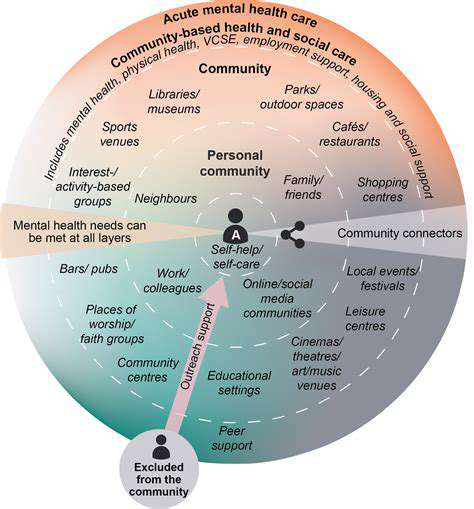
Building an effective predictive system requires gathering information from multiple channels. Beyond standard clinical data, valuable insights come from parent surveys, caregiver notes, and broader contextual details like neighborhood characteristics. This multifaceted approach provides a richer understanding of each individual's situation.
Building and Testing Predictive Systems
Creating reliable predictive tools involves thoughtful selection of relevant factors and application of advanced computational methods. Techniques like regression studies and classification models are commonly used. Thorough testing against independent datasets remains essential to verify the system's ability to forecast outcomes accurately.
Resource Management Implications
These analytical approaches can revolutionize how support services distribute their resources. By identifying children most likely to require assistance, programs can allocate their staff and materials more efficiently, decreasing waiting periods and enhancing intervention effectiveness. This focused strategy helps ensure vital services reach those with the greatest need.
Sophisticated modeling techniques enable support programs to maximize their limited resources. By concentrating on higher-risk cases, these initiatives can direct their efforts where they'll make the most significant difference.
Ethical Questions and Privacy Protection
Implementing predictive analytics in early support programs brings important ethical considerations about information security and possible systemic biases. Maintaining strict confidentiality for sensitive personal details remains crucial. Additionally, the development and application of these models require careful examination to prevent any unfair or prejudicial results.
Balancing universal access to early support services with robust data protection measures represents a critical challenge in implementing predictive analytics. Special attention must be paid to identifying and correcting any biases in the data or models to prevent unequal treatment.
Emerging Trends and Ongoing Studies
Additional research will help improve predictive models and extend their use to various populations. Incorporating new technologies like wearable monitors and cutting-edge analysis methods shows particular promise for enhancing the precision and practicality of early support efforts. Examining the long-term effects of interventions suggested by these models also deserves attention.
Ongoing investigation and refinement of predictive analytics for early intervention remain vital for improving accuracy and reducing potential biases. Exploring novel data streams and enhancing models will produce more reliable predictions and better-targeted support strategies.
Customized Care Approaches

Tailored Care Strategies for Better Results
Developing individualized care plans represents a fundamental shift toward more effective treatment. Customized approaches account for each patient's unique situation, incorporating their health background, daily routines, and personal choices. This personalized method increases the chances of positive outcomes while reducing unwanted effects.
When healthcare providers understand the complete picture of an individual's circumstances, they can create strategies that target underlying issues rather than just managing symptoms. This comprehensive perspective frequently leads to more durable improvements in health and daily functioning.
Comprehensive Patient Assessment
Successful customized care begins with detailed evaluation of the patient's specific requirements. This thorough examination should encompass their medical background, current concerns, lifestyle patterns, and personal objectives. Collecting this detailed information enables healthcare teams to design care plans that target core issues, moving beyond simple symptom management.
These evaluations often explore daily habits, nutritional patterns, and emotional health. Considerations like stress management, sleep quality, and social connections play important roles, as these factors significantly influence treatment effectiveness.
Creating Detailed Care Plans
After completing a comprehensive assessment, healthcare providers can develop a detailed care strategy. This plan should specify concrete actions, measurable goals, and realistic timelines. The strategy must align with the patient's individual circumstances and preferences, ensuring it's both practical and maintainable over time.
Effective plans also include provisions for regular progress reviews and necessary modifications. This flexible approach allows for adjustments as the patient's needs change throughout their care journey.
Tracking Progress and Refining Approaches
Continual monitoring remains essential for maintaining treatment effectiveness and relevance. Scheduled follow-ups let healthcare providers evaluate the patient's response to treatment, spot any new concerns, and refine the care plan accordingly. This ongoing evaluation process helps ensure the treatment remains appropriate and beneficial at every stage.
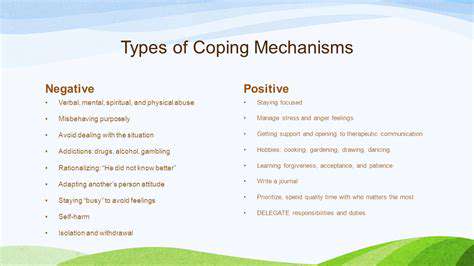
Anticipating Potential Difficulties
Well-designed customized care plans should proactively identify and prepare for possible challenges during treatment. Planning for potential obstacles enables early response and reduces the likelihood of treatment interruptions. This proactive stance proves invaluable for keeping patients motivated and maintaining treatment momentum.
Addressing potential challenges typically involves preparing strategies for handling side effects, developing coping skills, and establishing strong support networks around the patient.
Encouraging Patient Participation
Active patient involvement and commitment represent critical success factors for any customized care plan. Including patients in plan development and implementation builds their sense of investment and accountability, strengthening their dedication to the process and improving overall results.
Clear explanations, thorough education, and consistent support give patients the tools they need to take an active role in their care. This collaborative relationship between patient and provider forms the foundation for lasting success.
Ethical Implications and Future Developments
Information Protection Measures
Maintaining strict information security represents a critical concern in all healthcare applications, particularly in sensitive areas like addiction treatment. Advanced encryption methods, controlled access systems, and data anonymization procedures help prevent unauthorized viewing, security incidents, or improper use of private details. This includes adhering to established privacy standards such as HIPAA (in the United States) and GDPR (in Europe), along with implementing clear policies regarding information retention to protect patient confidentiality and preserve trust. Neglecting these safeguards could lead to serious consequences, from legal penalties to damaged reputations and potential harm to those seeking treatment.
Implementing robust security protocols does more than prevent data incidents; it also helps build patient confidence. Being transparent about how information gets used, obtaining proper consent, and clearly explaining protective measures all contribute to creating a safe environment for individuals receiving care.
Addressing Algorithmic Fairness
Since AI systems learn from existing data, they risk perpetuating any biases present in that information when making treatment suggestions or evaluations. For example, if certain demographic or socioeconomic groups appear disproportionately in the training data, the system might make unfair judgments about individuals from under-represented backgrounds, possibly leading to incorrect assessments or unsuitable treatment recommendations. Thoughtful planning and active measures become necessary to guarantee fair and equitable application of AI in addiction treatment.
Tackling algorithmic bias requires multiple strategies. These include using diverse and representative datasets, conducting regular bias audits of AI systems, and continuously monitoring their effects across different patient groups. Human oversight also plays a crucial role in ensuring responsible and ethical AI use, helping identify and correct biases when they occur.
Clear Decision-Making Processes
Both patients and clinicians need to comprehend how AI systems reach their conclusions. Without this understanding, trust suffers and identifying potential mistakes or biases becomes difficult. Explainable AI methods help make AI decision processes understandable to healthcare providers and patients alike, allowing them to follow the reasoning behind treatment suggestions. This clarity fosters trust and strengthens the therapeutic relationship.
Creating understandable AI models proves essential for establishing trust and accountability. When AI recommendations come with clear explanations, clinicians can better evaluate and adapt them for individual patients. This approach encourages more collaborative and effective treatment. Being open about AI capabilities and limitations also remains important.
Emerging Opportunities and Research Focus
AI applications in addiction treatment represent a relatively new field with significant potential for growth. Future studies should concentrate on developing more advanced AI models capable of creating personalized treatment plans, predicting relapse risks, and identifying high-risk individuals earlier. Additionally, successfully integrating AI into current healthcare frameworks and designing intuitive interfaces will be key for broad adoption and successful implementation.
Long-term studies examining the effectiveness and lasting impact of AI-assisted treatment also merit attention. Such research will help assess different AI approaches and uncover any unintended consequences. Cooperation between AI specialists, clinicians, and policy makers remains essential to ensure ethical and responsible AI use in treating substance use disorders. Ethical considerations must guide all future development efforts in this field.
Read more about AI in Substance Abuse Treatment: Personalized Recovery Paths
Hot Recommendations
- AI Driven Personalized Sleep Training for Chronic Insomnia
- AI Driven Personalization for Sustainable Stress Management
- Your Personalized Guide to Overcoming Limiting Beliefs
- Understanding Gender Dysphoria and Mental Health Support
- The Power of Advocacy: Mental Health Initiatives Reshaping Society
- Building a Personalized Self Compassion Practice for Self Worth
- The Ethics of AI in Mental Wellness: What You Need to Know
- AI Driven Insights into Your Unique Stress Triggers for Personalized Management
- Beyond Awareness: Actionable Mental Health Initiatives for Lasting Impact
- Creating a Personalized Sleep Hygiene Plan for Shift Workers