Personalized Mental Health: The Human Element in an AI World
The Potential for Personalized Treatment
Modern mental health care stands at the brink of transformation through artificial intelligence, which enables customized treatment strategies designed for individual circumstances. By examining extensive collections of patient records, symptoms, and treatment outcomes, advanced computational systems can detect trends and forecast potential results more precisely than conventional approaches. This facilitates more targeted interventions, potentially shortening the duration required for diagnosing and addressing mental health concerns.
Consider a framework capable of predicting which therapeutic method would most likely benefit a specific individual based on their distinctive traits and past encounters. Such tailored solutions could yield better treatment results and foster a more patient-focused healthcare paradigm.
Improving Accessibility and Affordability
Among the most notable advantages of AI in mental health services is its capacity to broaden care availability, especially in resource-limited regions. Automated conversational agents and digital helpers can offer preliminary assistance and evaluation, enabling people to connect with suitable resources more easily. This proves particularly valuable in locations with scarce mental health specialists.
Moreover, intelligent automation tools may help decrease mental health service expenses. By handling routine administrative functions and providing on-demand support, these systems can streamline healthcare processes, making psychological services more economical and attainable for diverse populations.
Enhanced Diagnostic Capabilities
Computational models can process multiple data types, including written communication, physiological measurements, and even facial cues, to spot subtle indicators of mental health challenges. This sophisticated analysis capacity might enable earlier intervention and more precise diagnoses, particularly in situations where traditional approaches might miss the complexities of a patient's condition.
The ability of machine learning to interpret intricate datasets could reveal novel risk factors and markers for psychological disorders, creating opportunities for preventive strategies and better long-term patient outcomes.
Addressing Bias and Ensuring Ethical Use
While AI offers substantial mental health benefits, we must confront potential algorithmic prejudices that might reinforce existing disparities and produce incorrect or unjust evaluations. Meticulous development and thorough validation are imperative to guarantee that intelligent tools operate fairly, justly, and with respect for personal needs and cultural backgrounds.
The Role of Human Interaction in the AI Era
Despite AI's potential, we must recognize that human connection remains essential in psychological care. Digital tools can serve as valuable supplements, offering support and guidance, but they cannot substitute the compassion, comprehension, and personalized attention that human therapists provide. An integrated methodology combining technological assistance with professional expertise appears most promising.
The Future of Personalized Mental Health
AI-enhanced personalized mental healthcare presents exciting possibilities for improving therapeutic results. As technology progresses, we anticipate increasingly advanced solutions aimed at enhancing availability, cost-effectiveness, and service quality. However, we must prioritize ethical considerations, ensuring these powerful tools serve individuals' welfare responsibly.
This will likely necessitate continuous investigation, innovation, and cooperation among AI experts, mental health practitioners, and patients to guarantee beneficial, equitable technology applications.
Overcoming Challenges and Ensuring Patient Safety
Implementing AI in psychological services presents unique obstacles. Protecting information confidentiality and security remains paramount, requiring strong safeguards. Additionally, we must ensure appropriate, ethical tool usage to prevent potential harm. Constant assessment is vital for recognizing and addressing any negative consequences.
Individuals must maintain control over their personal data and comprehend how intelligent systems utilize it. Open communication and clarity are fundamental for establishing trust and empowering those seeking psychological support.
Tailoring Treatment Plans: AI as an Assistant, Not a Replacement

Leveraging AI for Personalized Medicine
Artificial intelligence is dramatically altering healthcare, enabling more precise, individualized treatment strategies. Computational models can process comprehensive patient information, including medical backgrounds, genetic tendencies, and lifestyle elements, to identify patterns and predict personal responses to various therapies. This capacity for customization represents a major advancement, promising better outcomes and fewer complications.
Predictive Modeling for Treatment Success
AI-powered predictive analytics can assess patient information to determine factors linked with therapeutic success or failure. This allows medical professionals to make better-informed treatment decisions, potentially leading to more effective interventions from the beginning. By anticipating possible difficulties, preemptive approaches can be employed, optimizing the chance of successful results.
Analyzing Imaging Data for Accurate Diagnoses
Machine learning excels at interpreting medical imagery such as X-rays, CT scans, and MRIs. This capability enables faster, more accurate diagnoses, permitting timely treatment and potentially halting disease progression. The speed and precision of AI in image analysis represents a transformative development in medical practice, resulting in superior patient outcomes.
Optimizing Drug Dosage and Timing
Intelligent systems can evaluate patient data to fine-tune medication amounts and schedules, minimizing adverse effects while maximizing therapeutic benefits. This individualized method ensures patients receive optimal medication quantities at the right times, enhancing treatment effectiveness. Such personalization constitutes a critical component of customized treatment planning.
Identifying Potential Drug Interactions
Computational algorithms can detect possible medication conflicts that might escape human notice. By highlighting these interactions, AI helps prevent negative reactions and ensures patient protection. This proactive stance reduces complication risks and improves overall treatment safety.
Monitoring Patient Response to Treatment
AI can continuously track how patients respond to therapy, permitting adjustments when necessary. Real-time data interpretation enables healthcare providers to identify unexpected responses and modify treatment plans accordingly. This dynamic methodology guarantees patients receive optimal care throughout their treatment.
Improving Access to Specialized Care
Intelligent tools may enhance specialized care access by aiding diagnosis and treatment planning. This proves especially valuable for patients in remote locations or those with limited specialist availability. By bridging geographic and resource divides, AI can democratize premium healthcare access, fostering more equitable opportunities for all populations. Ultimately, this will enhance overall public health.
The Ethical Considerations of AI in Mental Health
Bias and Fairness in AI Systems
AI models learn from data, and if that information reflects societal prejudices, the systems will likely perpetuate and intensify those biases. This can produce unjust or discriminatory results in areas like financial services, employment screening, and legal proceedings. Mitigating these biases demands careful data selection and algorithm construction, ensuring impartiality and fair representation in training materials. This crucial challenge requires persistent research and proactive solutions.
Transparency and Explainability in AI
Many AI systems, particularly complex neural networks, function as opaque mechanisms, making their decision processes difficult to comprehend. This opacity complicates error identification and bias detection, potentially undermining public confidence. Creating more transparent and interpretable AI systems is essential for maintaining accountability and enabling human supervision. This includes developing methods to visualize decision pathways and provide clear rationales for AI conclusions.
Job Displacement and the Future of Work
AI's automation potential raises concerns about employment impacts across multiple industries. While creating new roles, AI may also displace workers performing repetitive tasks or data analysis. Workforce preparation through education and retraining initiatives is crucial to minimize potential social disruption. This includes cultivating skills that complement rather than compete with AI capabilities.
Privacy and Data Security in AI
AI systems frequently depend on extensive personal data collections, raising significant confidentiality concerns. Information breaches and misuse present serious dangers, necessitating stringent protective measures for sensitive data. Ethical standards and regulations are vital to ensure responsible data gathering, storage, and utilization in AI development. Maintaining individual control over personal information remains essential.
Accountability and Responsibility in AI Development
Determining liability when AI systems err or cause harm presents complex challenges. Establishing clear responsibility frameworks for AI creators, implementers, and users is necessary for risk mitigation. This includes formulating ethical guidelines, professional standards, and robust oversight mechanisms. Developing structures to address AI-related harm remains a significant undertaking.
The Impact of AI on Human Values and Society
AI's rapid development prompts fundamental questions about work nature, human relationships, and societal evolution. Considering AI's broader societal implications is critical to ensure its advancement aligns with human principles and promotes justice and equality. Ongoing dialogue and cooperation between technologists, policymakers, and the public are crucial for navigating forthcoming ethical challenges.
The Future of Personalized Mental Health: A Collaborative Approach
Personalized Mental Health Strategies
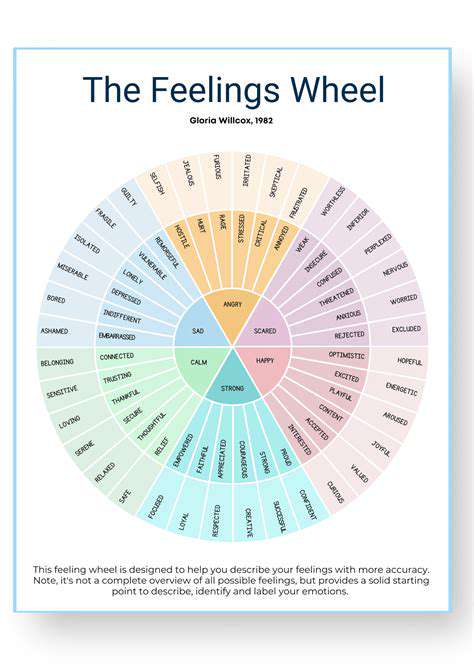
The psychological healthcare landscape is clearly shifting toward individualized methodologies. Moving beyond standardized treatment models, clinicians increasingly acknowledge each person's unique needs and experiences. This personalized perspective recognizes that mental health conditions involve complex interactions between genetic, environmental, and personal historical factors. Adapting interventions to specific patient requirements, preferences, and objectives leads to more effective, sustainable results.
This personalized shift demands deeper patient understanding. Comprehensive data collection, including medical histories, lifestyle factors, and personal narratives, proves essential for developing truly impactful treatment plans. This evidence-based methodology can substantially enhance diagnostic accuracy and therapeutic efficiency.
Technology's Role in Personalized Mental Health
Emerging digital solutions are transforming personalized mental healthcare delivery. Mobile applications, wearable technology, and intelligent tools provide readily available resources, assistance, and monitoring. These innovations can deliver customized feedback, tailored exercises, and early intervention tactics, significantly expanding care access, particularly in underserved areas.
Telemedicine platforms are already revolutionizing psychological services, enabling remote connections between individuals and therapists. This accessibility broadens treatment possibilities for those facing geographic barriers or lacking in-person service options. Technology integration also permits continuous mental wellness monitoring, facilitating more proactive, responsive care.
Collaborative Care Models
Truly personalized approaches require cooperation among multiple stakeholders, including clinicians, patients, family members, and support networks. Open dialogue and shared decision-making are critical to ensure treatment plans align with individual objectives and values. This cooperative model promotes shared responsibility and empowers patients to actively engage in their recovery processes.
Data Privacy and Security Concerns
As personalized mental health increasingly relies on technology and data collection, protecting patient confidentiality becomes paramount. Robust security protocols and transparent data management practices are essential for safeguarding sensitive information. Clear guidelines and regulations regarding data usage and access are vital for building trust and maintaining treatment integrity.
The Importance of Cultural Sensitivity
Recognizing and addressing diverse cultural backgrounds proves crucial for effective personalized mental healthcare. Psychological conditions may manifest differently across cultures, necessitating culturally appropriate treatment approaches. Healthcare providers require training to understand and address various cultural needs, ensuring both effective and respectful care.
Addressing the Cost and Accessibility of Care
Ensuring equitable access to personalized mental healthcare presents significant challenges. Advanced diagnostic tools and customized interventions may prove cost-prohibitive for some individuals. Innovative financing models or government support could make these services more affordable and accessible, maximizing personalized approach benefits. Expanding affordable mental healthcare access remains essential for promoting psychological well-being across society.
Read more about Personalized Mental Health: The Human Element in an AI World
Hot Recommendations
- AI Driven Personalized Sleep Training for Chronic Insomnia
- AI Driven Personalization for Sustainable Stress Management
- Your Personalized Guide to Overcoming Limiting Beliefs
- Understanding Gender Dysphoria and Mental Health Support
- The Power of Advocacy: Mental Health Initiatives Reshaping Society
- Building a Personalized Self Compassion Practice for Self Worth
- The Ethics of AI in Mental Wellness: What You Need to Know
- AI Driven Insights into Your Unique Stress Triggers for Personalized Management
- Beyond Awareness: Actionable Mental Health Initiatives for Lasting Impact
- Creating a Personalized Sleep Hygiene Plan for Shift Workers