AI for Eating Disorders: Personalized Digital Support for Recovery
Accessibility and Affordability: Expanding Access to Care
AI-Powered Tools for Enhanced Accessibility
Artificial intelligence (AI) is revolutionizing healthcare accessibility, particularly in the realm of mental health. AI-powered chatbots and virtual assistants can provide immediate, 24/7 support for individuals struggling with eating disorders, offering crucial initial guidance and emotional support when access to traditional therapy might be limited by geography, cost, or scheduling constraints. These tools can also be programmed to recognize and respond to specific warning signs, facilitating early intervention and potentially preventing escalation of symptoms.
Furthermore, AI algorithms can analyze vast amounts of data to identify patterns and risk factors associated with eating disorders, allowing for more personalized and proactive interventions. This personalized approach can lead to more effective treatment plans tailored to individual needs, thereby improving outcomes and expanding access to care for those who might otherwise have limited options.
Affordability through Scalable Solutions
One of the significant barriers to accessing quality eating disorder care is the often prohibitive cost. AI-driven platforms can significantly reduce these costs by providing scalable and accessible solutions. These platforms can offer a tiered system of care, ranging from basic information and support resources to more intensive, virtual therapy sessions, making treatment more affordable for a wider range of individuals.
By automating certain aspects of care, such as scheduling and basic assessments, AI can decrease the overall cost of treatment. This allows for greater investment in the personalized aspects of care, potentially leading to more effective interventions and better outcomes.
Personalized Treatment Plans via AI
AI algorithms can analyze individual patient data, including medical history, lifestyle factors, and emotional responses, to develop highly personalized treatment plans. This approach takes into account the unique needs and challenges of each individual, ensuring that interventions are targeted and effective. Through continuous monitoring and adaptation, these AI-driven plans can be adjusted based on the patient's progress and evolving needs, leading to more dynamic and effective treatment strategies.
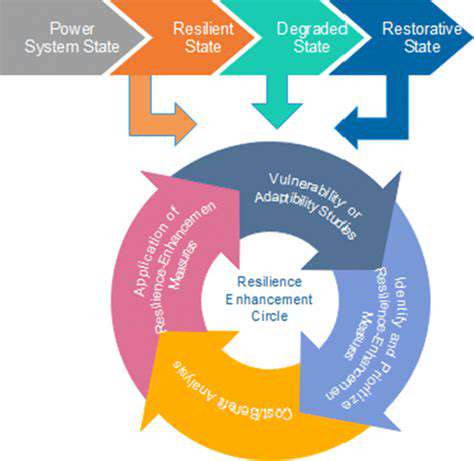
AI-Supported Remote Monitoring and Support
Remote monitoring and support are crucial for individuals with eating disorders, particularly those living in underserved areas or facing logistical challenges. AI-powered applications can track key metrics, such as food intake, weight, and mood, providing valuable data for clinicians and patients alike. This continuous monitoring allows for early detection of potential relapses or worsening symptoms, enabling timely interventions and adjustments to treatment plans.
AI-supported remote support groups and virtual therapy sessions can also connect individuals with a wider network of peers and professionals, fostering a sense of community and providing crucial social support, which is often a critical component of recovery.
Enhanced Early Detection and Prevention
AI algorithms can analyze large datasets of patient information to identify patterns and risk factors associated with eating disorders, enabling the development of predictive models. These models can help identify individuals at high risk of developing an eating disorder, facilitating early intervention and preventative measures. Early detection and intervention are crucial in improving outcomes and preventing long-term complications.
By identifying potential warning signs and risk factors early on, AI can help pave the way for timely interventions, ultimately improving the overall well-being of individuals and families affected by eating disorders.
Ethical Considerations and Future Directions
As AI technologies become increasingly integrated into eating disorder care, it's crucial to address the ethical implications. Data privacy, algorithmic bias, and the potential for over-reliance on technology are among the critical considerations. Ongoing research and development are needed to ensure that AI tools are deployed responsibly and ethically, safeguarding patient well-being and promoting transparency and accountability.
Future research should focus on developing AI systems that are not only effective but also culturally sensitive and inclusive, ensuring equitable access to care for all individuals, regardless of their background or socioeconomic status. A collaborative approach involving clinicians, researchers, and patients is essential to shape the future of AI in eating disorder care.
Read more about AI for Eating Disorders: Personalized Digital Support for Recovery
Hot Recommendations
- AI Driven Personalized Sleep Training for Chronic Insomnia
- AI Driven Personalization for Sustainable Stress Management
- Your Personalized Guide to Overcoming Limiting Beliefs
- Understanding Gender Dysphoria and Mental Health Support
- The Power of Advocacy: Mental Health Initiatives Reshaping Society
- Building a Personalized Self Compassion Practice for Self Worth
- The Ethics of AI in Mental Wellness: What You Need to Know
- AI Driven Insights into Your Unique Stress Triggers for Personalized Management
- Beyond Awareness: Actionable Mental Health Initiatives for Lasting Impact
- Creating a Personalized Sleep Hygiene Plan for Shift Workers