AI Driven Personalized Therapies for PTSD: New Frontiers
Personalized Treatment Plans
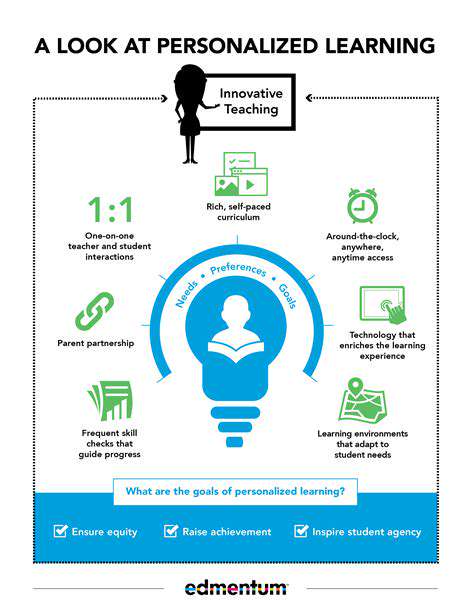
Artificial intelligence (AI) is revolutionizing healthcare, and PTSD treatment is no exception. By analyzing patient data, including symptoms, medical history, and even lifestyle factors, AI algorithms can create highly personalized treatment plans. This personalized approach goes beyond a one-size-fits-all approach, addressing the unique needs of each individual suffering from PTSD. These plans can be dynamic, adapting to changes in a patient's condition and ensuring that the most effective interventions are consistently applied. This level of customization can significantly improve treatment outcomes and patient satisfaction.
Moreover, AI-powered platforms can provide patients with tailored resources and support. This includes access to relevant articles, educational materials, and even virtual support groups. These resources can empower patients to take an active role in their recovery journey, fostering a sense of ownership and agency. This increased engagement can lead to faster progress and sustained improvements over time.
Enhanced Accessibility and Affordability
Traditional PTSD treatment often faces challenges with accessibility and affordability. Geographical limitations, long wait times for appointments, and the high cost of therapy can make it difficult for many individuals to access the help they need. AI-driven solutions can potentially address these challenges. Virtual therapy platforms, powered by AI, can offer convenient and accessible treatment options, particularly for those in remote areas or with limited mobility.
Furthermore, AI can potentially reduce the cost of treatment. By automating certain tasks, such as scheduling appointments and providing basic support, AI can free up therapists' time, allowing them to focus on more complex cases and potentially reducing the overall cost of care. This increased accessibility and affordability is crucial for ensuring that a broader population can benefit from effective PTSD treatments.
Improved Treatment Outcomes and Monitoring
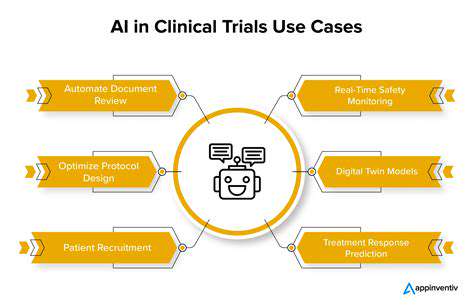
AI's ability to analyze vast amounts of data allows for a more comprehensive understanding of PTSD. By tracking patient progress over time, AI can identify patterns and potential triggers, providing valuable insights for therapists. This data-driven approach can lead to more effective treatment strategies, allowing therapists to adapt their interventions as needed. This constant monitoring and adaptation can significantly improve the overall effectiveness of PTSD treatment.
Furthermore, AI can aid in identifying individuals at risk of developing PTSD. By analyzing factors such as exposure to traumatic events and pre-existing conditions, AI systems can flag individuals who may need early intervention. This proactive approach can prevent the progression of PTSD and improve long-term outcomes. Early intervention is critical in mitigating the long-term impact of PTSD, and AI can be an invaluable tool in achieving this goal.
AI's Role in Assessing and Diagnosing PTSD
AI's Role in Disease Assessment
Artificial intelligence (AI) is rapidly transforming healthcare, offering innovative solutions for disease assessment and diagnosis. AI algorithms can analyze vast datasets of medical images, patient records, and genetic information to identify patterns and anomalies that might be missed by human clinicians. This ability to process information at scale allows AI to assist in earlier and more accurate diagnoses, potentially leading to improved patient outcomes.
By identifying subtle patterns and correlations in medical data, AI can flag potential issues that might otherwise remain undetected. This early detection is crucial in many diseases, allowing for timely interventions and potentially preventing the progression of serious conditions.
Improving Diagnostic Accuracy
One of the key benefits of AI in healthcare is its potential to improve diagnostic accuracy. AI algorithms can be trained on large datasets of medical images and patient data, enabling them to learn the subtle features that indicate a particular disease. This allows for a more objective and potentially more accurate assessment compared to purely human-driven diagnostics.
AI-powered diagnostic tools can analyze images with a level of detail and speed that surpasses human capabilities. This heightened precision can lead to earlier and more accurate diagnoses, potentially reducing the need for invasive procedures and improving overall patient care.
Automation of Routine Tasks
AI can automate many routine tasks in healthcare, freeing up clinicians to focus on more complex cases. For example, AI can analyze medical images, such as X-rays and CT scans, to identify potential abnormalities. This allows radiologists to review the results more efficiently, allowing them to focus on cases that require their expertise.
Personalized Treatment Strategies
AI has the potential to personalize treatment strategies by analyzing individual patient data. By considering factors like genetic makeup, lifestyle, and medical history, AI can help tailor treatment plans to maximize effectiveness and minimize side effects. This personalized approach can lead to improved outcomes and reduced healthcare costs.
Ethical Considerations and Future Directions
Despite the numerous benefits, the use of AI in healthcare also raises important ethical considerations. Issues such as data privacy, algorithmic bias, and the responsibility for AI-driven diagnoses need careful consideration and regulatory frameworks.
The future of AI in healthcare is promising, with ongoing research and development focused on improving the accuracy, reliability, and ethical implementation of AI-powered diagnostic tools. As technology advances, we can anticipate even greater integration of AI into healthcare systems, leading to more efficient, personalized, and effective patient care.
Personalized Treatment Plans: Tailoring Interventions to Individual Needs

Personalized Treatment Plans: Tailored Approaches for Optimal Outcomes
Personalized treatment plans are becoming increasingly important in healthcare, moving away from a one-size-fits-all approach. This shift recognizes that individual patients have unique needs, genetic predispositions, and responses to various therapies. By considering these individual factors, healthcare providers can develop strategies that are more likely to be effective and less prone to adverse effects. This approach is particularly crucial in chronic conditions where long-term management is vital.
These plans go beyond simply adjusting dosage or medication. They incorporate lifestyle modifications, dietary recommendations, and other non-pharmaceutical interventions tailored to the patient's specific situation. This holistic approach aims to address the root causes of the condition and promote overall well-being.
Gathering Comprehensive Patient Data
A crucial first step in creating a personalized treatment plan is gathering comprehensive patient data. This includes not only medical history, but also lifestyle factors, dietary habits, and social support networks. Understanding these aspects provides a more complete picture of the patient as a whole, allowing for a more nuanced and effective treatment strategy.
Accurate and detailed data is essential for identifying potential risk factors and tailoring interventions that are most likely to yield positive results. This data collection process should also involve open communication and collaboration with the patient to ensure their active participation in the plan's development.
Considering Genetic Predispositions
Advances in genomics have allowed healthcare professionals to incorporate genetic predispositions into personalized treatment plans. This information can reveal genetic variations that may influence how a patient responds to certain medications or therapies. Identifying these variations is crucial for selecting the most appropriate treatment options and potentially preventing adverse reactions.
For example, knowledge of specific genetic markers can help determine the likelihood of a patient experiencing drug toxicity or the effectiveness of a particular cancer treatment. This level of precision can significantly enhance the likelihood of positive outcomes.
Incorporating Lifestyle Factors
Personalized treatment plans often incorporate lifestyle modifications as a key component. These modifications may include dietary recommendations, exercise routines, stress management techniques, and sleep hygiene practices. Integrating these lifestyle factors into the treatment plan can significantly improve overall health and well-being, contributing to a more sustainable and effective therapeutic approach.
Tailoring these lifestyle modifications to the individual's preferences and current habits is crucial for ensuring adherence and long-term success. It's important to create a personalized plan that is realistic and achievable for the patient.
Monitoring and Adjusting the Plan
A personalized treatment plan is not a static document. It requires ongoing monitoring and adjustments based on the patient's response and evolving needs. Regular check-ups, assessments, and feedback from the patient are essential to track progress and make necessary modifications.
By adapting the plan as needed, healthcare providers can ensure that it remains effective and relevant throughout the treatment process. This dynamic approach allows for a more responsive and personalized experience for each individual patient.
Collaboration and Communication
Effective personalized treatment plans require strong collaboration between patients, healthcare providers, and other support systems. Open communication channels facilitate a shared understanding of the plan's goals and objectives. This collaborative approach ensures that all stakeholders are on the same page and working towards the same outcome.
Clear communication fosters trust and empowers patients to actively participate in their own care. It also allows for prompt identification of any challenges or roadblocks that may arise during the treatment process.
Patient Empowerment and Active Participation
Personalized treatment plans place a strong emphasis on patient empowerment and active participation. Patients are encouraged to take ownership of their health and actively engage in the development and execution of their treatment plan. This fosters a sense of responsibility and control, which can significantly enhance adherence and motivation.
Encouraging patient autonomy and active participation in decision-making is essential for promoting a positive and sustainable health outcome. This empowers patients to take an active role in their own care, leading to better health outcomes and a stronger sense of well-being.
AI-Enhanced Cognitive Behavioral Therapy (CBT) and Exposure Therapy
AI-Powered Personalized CBT
AI-enhanced CBT leverages machine learning algorithms to tailor treatment plans to individual patient needs. This personalized approach goes beyond generic protocols, dynamically adjusting interventions based on real-time data and feedback. By analyzing patient responses, emotional states, and behavioral patterns, AI can identify specific triggers and vulnerabilities, allowing therapists to focus on the most impactful areas for change. This targeted approach leads to more efficient and effective treatment outcomes.
The ability of AI to analyze vast datasets of patient information allows it to identify patterns and predict potential challenges. This proactive approach helps therapists anticipate potential obstacles and develop preventative strategies, leading to better patient engagement and improved long-term outcomes. Ultimately, personalized CBT, powered by AI, aims to provide a more dynamic and effective therapeutic experience.
Enhanced Exposure Therapy with AI
AI can significantly enhance exposure therapy by automating and optimizing exposure exercises. This includes generating tailored exposure hierarchies, selecting appropriate stimuli, and providing real-time feedback and support. AI can also measure the patient's emotional response during exposure, enabling a more precise and controlled approach to desensitization. This automation frees up therapists to focus on the patient's emotional regulation and overall well-being, potentially leading to faster and more effective progress.
Improving Accessibility and Affordability
AI-driven CBT and exposure therapy tools have the potential to increase accessibility to mental health services. By automating certain aspects of therapy, AI can make these services more affordable, potentially reducing the financial burden on patients and insurance providers. Remote delivery options enabled by AI can expand access to therapists in underserved areas and reduce travel costs and time constraints for patients.
Streamlined Treatment Processes
AI can streamline many aspects of CBT and exposure therapy, from scheduling appointments to monitoring progress. Automated reminders, personalized feedback systems, and progress tracking tools can significantly improve the efficiency of the entire treatment process. This streamlined approach allows therapists to dedicate more time to interacting with patients and building therapeutic relationships, fostering a more supportive and productive therapeutic environment. The automation of administrative tasks allows therapists to prioritize patient care.
Ethical Considerations and Future Directions
The integration of AI in mental health care presents important ethical considerations regarding data privacy, security, and the potential for bias in algorithms. Careful attention needs to be paid to ensuring patient data is protected and used responsibly. Future research should focus on developing robust ethical guidelines and frameworks for AI-assisted CBT and exposure therapy. The integration of AI should be approached with a focus on enhancing human therapists' skills and providing better support, rather than replacing them entirely.
Read more about AI Driven Personalized Therapies for PTSD: New Frontiers
Hot Recommendations
- AI Driven Personalized Sleep Training for Chronic Insomnia
- AI Driven Personalization for Sustainable Stress Management
- Your Personalized Guide to Overcoming Limiting Beliefs
- Understanding Gender Dysphoria and Mental Health Support
- The Power of Advocacy: Mental Health Initiatives Reshaping Society
- Building a Personalized Self Compassion Practice for Self Worth
- The Ethics of AI in Mental Wellness: What You Need to Know
- AI Driven Insights into Your Unique Stress Triggers for Personalized Management
- Beyond Awareness: Actionable Mental Health Initiatives for Lasting Impact
- Creating a Personalized Sleep Hygiene Plan for Shift Workers