AI Driven Insights into Your Genetic Predisposition for Mental Health
Compounding the issue, many algorithms are trained on datasets that overrepresent certain ethnic or socioeconomic groups. Such imbalances can distort outcomes, worsening rather than alleviating health disparities. Mitigating these biases demands thorough testing using diverse, representative data to validate AI models.
Protecting Patient Privacy and Data Security
Given the highly sensitive nature of genetic information, robust security protocols are essential. Implementing advanced encryption and strict access controls safeguards patient confidentiality, fostering trust and ensuring compliance with data protection laws.
Beyond technical safeguards, ethical obligations include transparent informed consent processes. Patients must fully grasp how their genetic data will be utilized, stored, and shared. Clear communication empowers individuals to make informed decisions about their personal information.
Ensuring Informed Consent and Transparency
AI-driven genetic analysis necessitates comprehensive consent procedures. Patients should be apprised of potential benefits, risks, and limitations, including implications for family members. Detailed explanations about data usage are fundamental to ethical practice.
Transparency extends to algorithmic development. Open access to AI models and underlying data promotes accountability. Explainable AI (XAI) techniques can demystify decision-making processes, enhancing trust in these technologies.
Addressing Accessibility and Cost Barriers
While AI-powered genetic insights promise healthcare revolutions, equitable access remains critical. Cost barriers and data access disparities must be addressed to ensure these advancements benefit all populations. Policy initiatives should aim to make testing and analysis more affordable and widely available.
The Vital Role of Genetic Counselors
Genetic counselors serve as indispensable guides through AI-driven genetic medicine. Their expertise in interpreting complex data and supporting patient decision-making ensures ethical considerations remain central to implementation.
These professionals bridge the gap between patients, healthcare providers, and technology, facilitating responsible use of genetic insights.
Future Implications and Directions
The convergence of AI and genetics presents both opportunities and challenges. Long-term impacts on health understanding and personalized medicine require ongoing evaluation. Evolving ethical frameworks must keep pace with technological advances through collaborative efforts across disciplines.
Personalized Strategies for Managing Potential Risks
Personalized Approaches to Stress Management
Effective stress management demands customization, as individual responses vary significantly. Identifying personal stressors through self-reflection forms the foundation of any successful strategy. For instance, work-related stress might require time management adjustments or colleague support systems.
Diverse techniques prove effective for different individuals. A blended approach incorporating mindfulness, physical activity, and other modalities often yields optimal results, with flexibility to adapt as circumstances change.
Customizing Techniques for Maximum Impact
Pinpointing stress triggers enables targeted intervention development. Social anxiety might benefit from communication skill-building, while physiological symptoms could respond to relaxation techniques like deep breathing.
Regular exercise offers dual benefits, releasing mood-enhancing endorphins while improving sleep quality. These physiological changes create a buffer against stress's physical manifestations.
Adapting Strategies Over Time
Effective stress management evolves with life changes. Major transitions like career shifts or personal milestones necessitate strategy reassessment to maintain effectiveness.
Periodic self-evaluation ensures continued relevance. This proactive approach guarantees strategies remain aligned with changing needs and circumstances.
Leveraging Support Systems
While personal strategies form the core, external support enhances effectiveness. Professional guidance offers specialized tools and objective perspectives when needed.
Therapists provide tailored coping mechanisms and insights that may elude self-assessment, particularly when stress significantly impacts daily functioning.
The Future of AI and Genetic Insights in Mental Health
AI-Powered Diagnostics Transforming Mental Healthcare
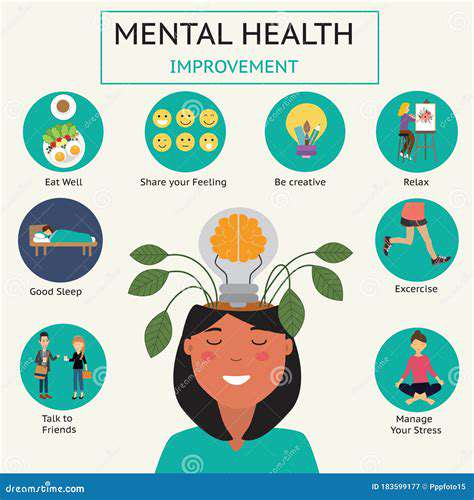
Artificial intelligence's healthcare revolution extends to mental health through comprehensive data analysis. AI's pattern recognition capabilities enable earlier, more accurate diagnoses, facilitating timely interventions that improve outcomes.
Machine learning excels at detecting subtle indicators often missed in traditional assessments. This precision proves invaluable for ambiguous symptoms or overlapping conditions, preventing symptom escalation through early detection.
Personalized Treatment Through Advanced Analytics
AI's analytical power facilitates truly individualized treatment plans. By synthesizing patient characteristics and treatment responses, algorithms can recommend optimized interventions.
Genetic Markers Illuminating Mental Health
Genetic research continues uncovering links between DNA and mental health conditions. Identifying susceptibility markers enables precision medicine approaches that target underlying biological mechanisms.
This molecular understanding informs preventative strategies while opening new research avenues. Genetic insights may eventually enable therapies addressing root causes rather than symptoms.
Synergizing AI and Genetic Data
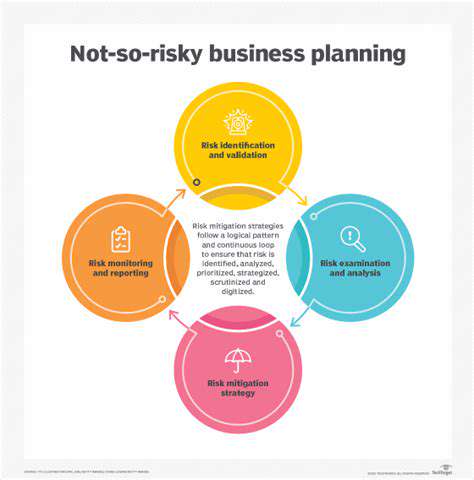
The combination of AI and genetic analysis creates powerful predictive tools. Early risk identification enables preventative measures, potentially reducing mental health burdens at individual and societal levels.
Navigating Ethical Challenges
These technological advances raise important ethical questions. Data privacy protections and equitable access must remain priorities to prevent exacerbating health disparities.
Expanding Access to Mental Healthcare
AI platforms and genetic insights promise to democratize mental healthcare. Digital tools can reach underserved populations, while personalized treatments may prove more cost-effective long-term.
Future Research Directions
Continued innovation requires refined diagnostic tools, personalized treatment algorithms, and robust ethical frameworks. Understanding gene-environment interactions will prove crucial for advancing mental healthcare.