Addressing Health Disparities: Equity Focused Mental Health Initiatives
Developing Culturally Competent Mental Health Services
Understanding Cultural Competence in Mental Health
Developing culturally competent mental health services is crucial for addressing health disparities. It necessitates a deep understanding of the diverse cultural backgrounds, beliefs, values, and experiences of individuals seeking mental health support. This understanding extends beyond surface-level awareness and requires a genuine commitment to recognizing and respecting the unique needs and perspectives of each client. Culturally competent providers must actively engage in continuous learning and self-reflection to improve their ability to provide effective and equitable care. This includes acknowledging the potential impact of cultural factors on mental health presentation and treatment adherence.
Cultural competence involves more than just knowing about different cultures. It also includes the ability to adapt one's approach to mental health care to meet the specific needs of each individual. This may involve incorporating culturally relevant communication styles, utilizing interpreters when necessary, and tailoring treatment strategies to align with the client's cultural values and beliefs. This approach fosters trust and rapport, essential components in building a strong therapeutic relationship.
Addressing Implicit Bias in Mental Health
Implicit bias, often unconscious, can significantly influence how mental health professionals interact with and treat clients from different cultural backgrounds. Recognizing and mitigating these biases is essential for creating equitable mental health services. This involves acknowledging that personal experiences and societal stereotypes can shape judgments and perceptions, potentially leading to misdiagnosis, inappropriate treatment recommendations, or unequal access to care. Training and ongoing education can help providers identify and challenge their own implicit biases to ensure fair and equitable treatment for all.
Tools and strategies for addressing implicit bias in mental health settings are vital. These tools can include self-reflection exercises, culturally sensitive training programs, and feedback mechanisms to promote continuous learning and improvement in cultural competence. These methods can make a significant difference in ensuring equitable access to and delivery of mental health services.
Culturally Sensitive Assessment and Diagnosis
Accurate assessment and diagnosis are fundamental to providing effective mental health care. However, cultural factors can significantly influence the presentation of mental health symptoms. A culturally sensitive assessment process should consider the client's cultural background, values, and beliefs when gathering information. This may involve using culturally appropriate assessment tools and exploring potential cultural influences on the client's experiences and behaviors. It is also crucial to avoid imposing Western diagnostic criteria without considering alternative perspectives and experiences.
Cultural considerations in diagnosis are particularly important. Mental health conditions may manifest differently across cultures, and symptoms that might be considered normal in one culture may be perceived as problematic in another. A culturally informed approach to assessment and diagnosis ensures that clients are understood within the context of their cultural background, leading to more accurate and appropriate diagnoses.
Developing Culturally Adapted Treatment Approaches
Effective treatment approaches must be tailored to the unique needs and cultural values of each individual. This means considering the client's preferences for communication styles, treatment modalities, and the involvement of family members or community support systems. Culturally adapted treatment plans can significantly enhance treatment outcomes by fostering trust, engagement, and a sense of cultural validation. This approach can lead to improved treatment adherence and better therapeutic outcomes.
Ensuring Equitable Access to Mental Health Services
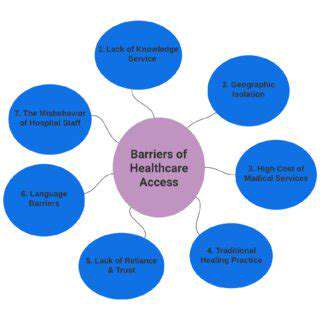
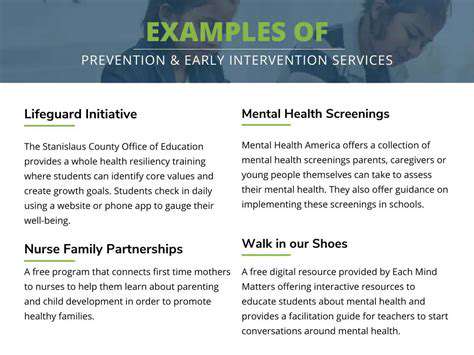
addressing health disparities requires ensuring equitable access to mental health services for all populations. This includes removing systemic barriers that disproportionately affect certain cultural groups, such as language barriers, geographic limitations, and financial constraints. Efforts to increase access to culturally competent providers and services can make a significant difference. Moreover, community-based mental health programs that incorporate culturally appropriate outreach strategies are essential for connecting individuals with resources and support.
Policies and programs that support the development of culturally competent mental health services are critical. These initiatives should prioritize culturally diverse staffing, promote culturally sensitive training and supervision, and invest in resources that support the delivery of equitable care. Addressing these systemic barriers is essential to achieving health equity in mental health.
Empowering Communities Through Advocacy and Collaboration
Building Trust and Understanding
Fostering trust between community members and healthcare providers is paramount in addressing health disparities. This requires active listening, cultural sensitivity, and a genuine commitment to understanding the unique needs and perspectives of diverse populations. Establishing open communication channels and actively involving community leaders and representatives in the planning and implementation of health initiatives is crucial for building a foundation of mutual respect and shared responsibility.
Open forums, community events, and focus groups can be invaluable tools for gathering information and ensuring that health programs are relevant and responsive to the specific concerns of those they serve. This proactive approach helps dispel misinformation and mistrust, creating a space where individuals feel empowered to seek and utilize healthcare services.
Addressing Systemic Barriers
Health disparities are often rooted in systemic issues such as socioeconomic factors, access to resources, and discriminatory practices. To effectively address these disparities, it's essential to identify and dismantle the underlying barriers that limit access to quality healthcare for vulnerable populations. This includes policies that promote equitable resource distribution, affordable housing initiatives, and programs designed to reduce poverty and food insecurity.
Collaboration between government agencies, community organizations, and healthcare providers is critical. By working together, these groups can develop comprehensive strategies to address the root causes of health disparities and create a more equitable healthcare system for everyone.
Promoting Health Literacy
Understanding health information and making informed decisions about one's health is crucial for everyone. However, health literacy levels vary significantly across communities, and this disparity can contribute to health disparities. Efforts to improve health literacy should be tailored to the specific needs of diverse populations, using accessible language, visual aids, and culturally appropriate formats.
Educational programs that teach individuals how to navigate the healthcare system, understand medical terminology, and interpret health information effectively can empower individuals to take control of their health. These programs can also promote healthy behaviors and reduce the risk of preventable diseases.
Encouraging Community Participation
Empowering communities to take ownership of their health is a key component of addressing health disparities. This involves fostering a sense of agency and responsibility within communities and providing opportunities for individuals to participate in health-related initiatives. Community gardens, health fairs, and educational workshops can serve as powerful platforms for fostering collaboration and promoting healthy lifestyles.
By giving individuals a voice and a role in shaping their health futures, they are more likely to actively engage in preventative measures, seek timely healthcare, and ultimately improve their overall health and well-being. This collaborative approach fosters a sense of collective responsibility and empowers individuals to become advocates for their own health.
Leveraging Technology for Access
Technology can play a significant role in bridging the gap in access to healthcare for underserved communities. Telemedicine platforms, mobile health applications, and online resources can make healthcare more accessible and convenient for those in rural areas or those with limited transportation options. These technologies can also improve communication between patients and providers, leading to better care coordination and improved health outcomes.
However, it's essential to consider the digital divide and ensure that technology solutions are culturally appropriate and accessible to all members of the community. Efforts to address health disparities must also recognize the importance of digital literacy and provide training and support for individuals who may lack access to technology or the skills to use it effectively.
Cultivating a Culture of Support
Addressing health disparities requires a fundamental shift in mindset, moving from a focus on individual deficits to a more holistic understanding of the interconnectedness of social determinants of health. Creating a supportive environment that promotes inclusivity, respect, and collaboration across all levels of society is essential for fostering equitable access to healthcare. This includes challenging harmful stereotypes, promoting cultural sensitivity, and fostering a sense of belonging among all community members.
Strong community networks and support systems can help individuals navigate complex healthcare systems and access the resources they need. Building a culture of support involves actively listening to the experiences of community members, responding to their needs with empathy, and creating opportunities for collaboration and mutual assistance.
Read more about Addressing Health Disparities: Equity Focused Mental Health Initiatives
Hot Recommendations
- AI Driven Personalized Sleep Training for Chronic Insomnia
- AI Driven Personalization for Sustainable Stress Management
- Your Personalized Guide to Overcoming Limiting Beliefs
- Understanding Gender Dysphoria and Mental Health Support
- The Power of Advocacy: Mental Health Initiatives Reshaping Society
- Building a Personalized Self Compassion Practice for Self Worth
- The Ethics of AI in Mental Wellness: What You Need to Know
- AI Driven Insights into Your Unique Stress Triggers for Personalized Management
- Beyond Awareness: Actionable Mental Health Initiatives for Lasting Impact
- Creating a Personalized Sleep Hygiene Plan for Shift Workers