AI for OCD: Innovative Digital Tools for Thought Management
Virtual Reality Exposure Therapy (VRET) is an innovative treatment approach using immersive virtual environments to help people confront and manage fears. This technique creates realistic simulations of anxiety-provoking situations, allowing gradual exposure in a safe setting. This process helps reduce sensitivity to triggers and develop coping strategies.
VRET proves especially effective for treating phobias, PTSD, and other anxiety conditions. It offers an engaging alternative to traditional exposure methods.
How It Works
VRET operates on gradual exposure principles. Patients encounter increasingly intense virtual scenarios related to specific fears. This controlled exposure helps reduce anxiety responses. By repeatedly facing fears in safe virtual settings, patients learn to manage reactions and build resilience.
Variety of Virtual Settings
VR environments vary widely, reflecting different anxiety types. From public speaking simulations to height or confined space scenarios, these immersive settings offer realistic, customizable experiences.
This customized approach enables highly personalized treatment plans for maximum effectiveness. It also provides a safe space to face fears without real-world consequences.
VRET Benefits
VRET's primary advantage is providing controlled exposure. This gradual approach minimizes potential for overwhelming experiences.
VRET often proves more engaging than traditional exposure, leading to quicker progress. The immersive nature typically increases patient involvement and motivation.
Comparing Traditional Methods
Traditional exposure therapy faces logistical challenges. Patients may struggle to access real-world exposure situations. VRET addresses these limitations through controlled, customizable experiences.
VRET offers flexibility in exposure intensity and duration, making it adaptable to diverse patients and conditions. This personalized approach often proves more efficient than traditional methods.
Effectiveness and Results
Research consistently demonstrates VRET's effectiveness for various anxiety disorders. Studies show significant symptom improvement following VRET interventions.
Positive outcomes often extend beyond treatment, leading to long-term quality of life improvements. VRET particularly benefits those who find traditional exposure too challenging.
Future Developments
VRET continues evolving, with research exploring new applications and technological advancements.
More research is needed to fully understand long-term effectiveness and optimal implementation strategies. VRET's potential to transform anxiety treatment is significant, with future developments promising enhanced outcomes.
Availability and Expansion of AI-Supported Treatment
Treatment Accessibility
AI-supported OCD treatment offers increased accessibility. Traditional therapy faces geographical, scheduling, and financial limitations. AI platforms overcome these through remote options, customized plans, and potentially lower costs. This accessibility is vital for underserved communities or those facing care access challenges.
AI can provide continuous support, offering help during anxiety spikes. This availability is crucial for OCD sufferers needing immediate assistance. Personalized plans tailored to individual needs further enhance accessibility.
Scalability Potential
AI-supported solutions scale effectively. Traditional therapy struggles with growing demand, while AI tools can expand across clinics, hospitals, and primary care settings. This scalability helps reach more OCD sufferers.
By automating certain tasks, AI frees therapist time for complex cases. This efficiency allows serving more patients, significantly increasing system capacity.
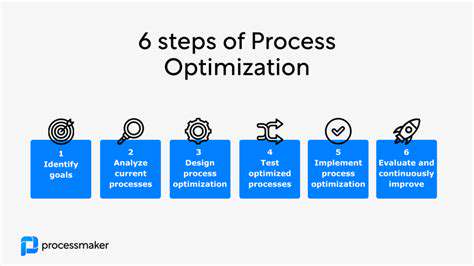
Customized Treatment Approaches
AI's data analysis enables highly personalized OCD treatment plans. These address specific symptoms, anxieties, and coping styles. Personalized approaches improve outcomes by ensuring relevance to individual needs. AI identifies behavioral patterns, allowing ongoing plan adjustments.
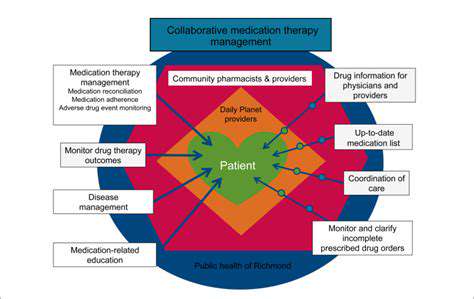
Healthcare System Integration
Successful AI treatment adoption requires seamless healthcare system integration. AI platforms should connect with electronic health records and clinical tools. This integration provides comprehensive patient history and progress data, enabling better provider collaboration and coordinated care.
Cost Efficiency
AI-supported treatment may cost less than traditional methods. Automation, reduced clinician time, and remote options can lower overall expenses. This affordability helps those facing financial barriers to mental healthcare.
Reducing Stigma, Improving Results
AI treatment can reduce mental health stigma. Accessible, convenient platforms encourage help-seeking without embarrassment. This can lead to earlier intervention and better outcomes. AI platforms' ease of use and privacy help remove care access barriers.
Ethical Aspects and Future Progress
While promising, AI treatment requires careful ethical consideration. Algorithm accuracy, potential data bias, and privacy protections need attention. Ongoing research ensures responsible AI implementation. Future advancements may include better diagnostic tools and personalized interventions, improving OCD treatment options.