AI for Bipolar Disorder: Managing Mood Swings with Smart Tools

Personalized Treatment Plans with AI Support
Personalized Treatment Plans with AI Support
AI-powered tools are revolutionizing the way we approach mental health treatment, offering the potential for more personalized and effective interventions. For bipolar disorder, this means tailoring treatment plans to the unique needs and patterns of each individual. These plans can be dynamic, adapting to changes in mood and symptom severity, providing a more proactive and responsive approach to managing this complex condition.
Data-Driven Insights for Enhanced Diagnosis
AI algorithms can analyze vast amounts of patient data, including medical history, symptom reports, and even social media posts (with appropriate ethical considerations), to identify subtle patterns and trends that might be missed by traditional diagnostic methods. This data-driven approach can lead to earlier and more accurate diagnoses, enabling timely intervention and potentially preventing severe mood episodes.
By identifying these patterns, AI can flag potential warning signs, allowing clinicians to intervene before a full-blown episode occurs. This proactive approach can significantly improve the quality of life for individuals living with bipolar disorder.
Predictive Modeling for Early Intervention
AI can be trained to predict potential mood swings and symptom exacerbations based on historical data. This predictive capability allows clinicians to anticipate challenges and proactively adjust treatment strategies before symptoms escalate. This proactive approach is invaluable in managing the unpredictable nature of bipolar disorder, potentially minimizing the severity and duration of manic or depressive episodes.
Automated Monitoring and Support Systems
AI-powered apps and wearable devices can provide continuous monitoring of mood, sleep patterns, and other relevant metrics. This real-time data can be used to inform treatment adjustments and provide tailored support to the patient, fostering greater self-awareness and promoting adherence to treatment plans. This continuous monitoring can also help identify patterns and triggers that might be contributing to mood instability.
Improved Medication Management and Adherence
AI can assist in optimizing medication regimens, predicting potential side effects, and prompting patients to take their medication as prescribed. This automated support can significantly improve medication adherence, a crucial factor in managing bipolar disorder effectively. Personalized medication schedules and reminders, tailored to individual needs, can dramatically enhance the effectiveness of treatment.
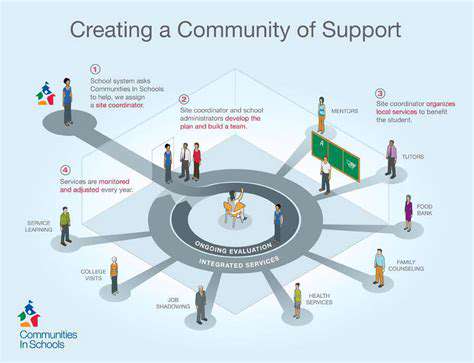
Enhanced Communication and Collaboration
AI tools can facilitate better communication between patients, healthcare providers, and support networks. This improved communication can lead to more comprehensive care and shared understanding of the patient's journey. Patients can access information and support resources more easily, fostering a collaborative approach to managing bipolar disorder. This integration of AI tools can break down barriers to effective communication.
Ethical Considerations and Future Directions
The integration of AI in mental health care requires careful consideration of ethical implications. Data privacy, algorithmic bias, and the potential for misinterpretation of results are crucial aspects to address. Ongoing research and development focusing on these ethical concerns will pave the way for responsible and beneficial applications of AI in bipolar disorder management. The future of AI in mental health care depends on a thoughtful and comprehensive approach to its development and implementation.
Real-Time Support and Emotional Intelligence
Real-Time Monitoring and Intervention
Real-time support systems, powered by AI, can continuously monitor individuals with bipolar disorder for subtle shifts in mood and behavior. This constant, almost imperceptible observation allows for rapid intervention before a full-blown manic or depressive episode takes hold. Such systems can analyze patterns in sleep, activity levels, social media interactions, and even physiological data like heart rate variability, providing early warning signs that a person might be heading towards a crisis. This proactive approach is vital for preventing severe episodes and improving overall quality of life.
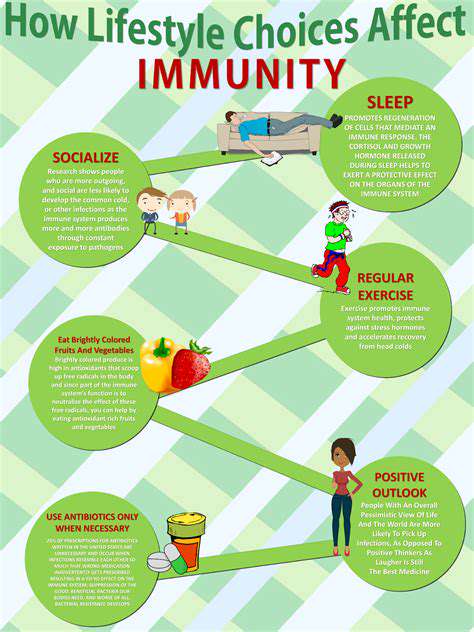
By leveraging machine learning algorithms, these AI-driven platforms can identify specific triggers associated with mood fluctuations in individual patients. This tailored understanding allows for targeted interventions, such as recommending specific coping mechanisms, suggesting lifestyle adjustments, or connecting the individual with appropriate support networks. The continuous nature of this monitoring, coupled with the ability to personalize interventions, provides a powerful tool for managing bipolar disorder proactively.
Emotional Intelligence and Personalized Support
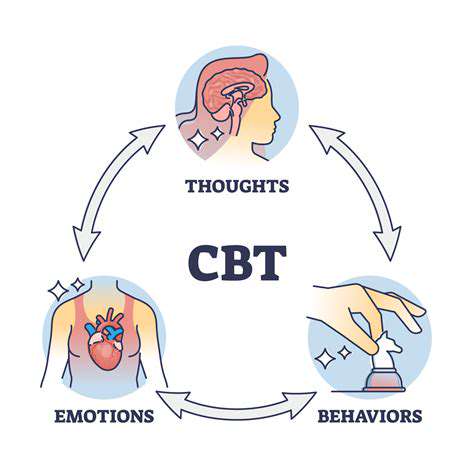
AI applications can be designed to act as virtual companions, offering emotional support and guidance. These AI-powered systems can analyze language patterns and tone in conversations, recognizing subtle indicators of distress, anxiety, or escalating emotions. Such systems can provide reassuring prompts, offer cognitive behavioral therapy techniques, and connect individuals with mental health professionals, all in real-time. This personalized support is crucial for managing the unpredictable nature of bipolar disorder.
Furthermore, these systems can adapt to individual needs and preferences. They can learn from past interactions and tailor their support accordingly. This personalized approach is especially valuable in addressing the unique emotional and social challenges that individuals with bipolar disorder often face. By providing a consistent, empathetic, and understanding presence, AI can significantly reduce feelings of isolation and enhance overall well-being.
Beyond providing emotional support, these AI tools can also promote self-awareness. By tracking patterns in mood and behavior, users can gain a deeper understanding of their own condition. This self-awareness is fundamental to managing bipolar disorder effectively, as it allows individuals to recognize triggers and develop strategies to cope with them. This empowerment is a crucial element of the overall management process.
The constant availability of these AI systems can be invaluable. Individuals struggling with bipolar disorder often face periods of heightened vulnerability, and having immediate access to support can make a significant difference in preventing crises and maintaining stability. This constant, available support system can potentially reduce the frequency and severity of episodes, leading to a more fulfilling and stable life for those affected.
Predictive Modeling for Proactive Management

Predictive Modeling Techniques
Predictive modeling, a crucial aspect of data science, leverages historical data to forecast future outcomes. This involves developing algorithms that analyze patterns and trends within the data to predict future behaviors or events. The goal is to identify potential opportunities and risks in advance, enabling proactive decision-making and improved outcomes. Various techniques exist, each with its strengths and weaknesses, including regression analysis, classification models, and time series forecasting.
Different predictive models cater to diverse needs. For example, regression models excel at predicting continuous variables, like sales figures or stock prices. Classification models, on the other hand, are ideal for predicting categorical variables, such as customer churn or product success. Choosing the right model depends significantly on the specific problem being addressed and the nature of the available data.
Proactive Applications in Business
Predictive modeling offers substantial benefits for businesses across various sectors. By anticipating potential problems or opportunities, companies can allocate resources more effectively and potentially avoid costly errors. For instance, identifying customer churn risk allows businesses to implement targeted retention strategies, ultimately boosting customer lifetime value.
Predictive modeling can also be used to forecast demand fluctuations. This forecasting capacity allows businesses to optimize inventory levels, minimize waste, and ensure product availability when and where it's needed. This proactive approach to inventory management directly impacts profitability and customer satisfaction.
Key Considerations in Implementation
Implementing predictive modeling requires careful consideration of several factors. Data quality is paramount; inaccurate or incomplete data will inevitably lead to unreliable predictions. Therefore, data cleaning and preprocessing steps are essential to ensure model accuracy and robustness.
Model selection and validation are equally critical. Choosing the appropriate model for the specific problem and validating its performance on unseen data are crucial steps to ensure the predictive model's effectiveness in real-world scenarios. This process minimizes the risk of overfitting, where the model performs well on the training data but poorly on new data.
Ethical Implications and Future Trends
As predictive modeling becomes more prevalent, understanding its ethical implications is essential. Bias in data can lead to discriminatory outcomes, so ensuring fairness and transparency in model development and deployment is paramount. Ethical considerations should be integrated into every stage of the process.
Future trends in predictive modeling include the increasing use of advanced machine learning algorithms, such as deep learning, and the integration of predictive modeling with other technologies like the Internet of Things (IoT) and big data analytics. These trends are likely to enhance the accuracy and scope of predictive modeling applications in various fields, offering more sophisticated and valuable insights.
Integrating AI into Existing Treatment Frameworks

Integrating AI into Existing Treatment Protocols
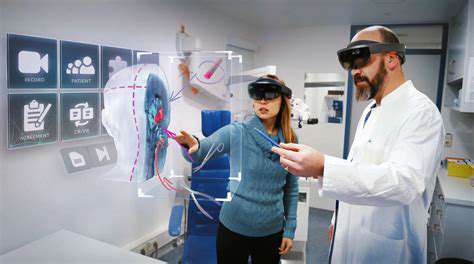
Integrating artificial intelligence (AI) into existing treatment protocols presents a significant opportunity to enhance patient care and improve clinical outcomes. AI algorithms can analyze vast amounts of patient data, including medical history, lab results, and imaging scans, to identify patterns and insights that might be missed by human clinicians. This data-driven approach can lead to more personalized and effective treatment strategies, ultimately benefitting patients.
Furthermore, AI can streamline administrative tasks, freeing up clinicians' time to focus on patient interaction and care. This efficiency boost allows for better allocation of resources and potentially reduces costs associated with healthcare delivery.
Challenges in Implementation
Despite the potential benefits, integrating AI into existing treatment protocols faces several challenges. One major hurdle is the need for robust and reliable data sets. AI algorithms require large quantities of high-quality data to learn and make accurate predictions. Ensuring data privacy and security is also crucial, particularly when dealing with sensitive patient information.
Another significant challenge lies in the need for appropriate infrastructure and expertise. Implementing AI systems requires specialized hardware and software, as well as skilled personnel to manage and maintain these systems. Integrating AI into existing workflows also necessitates training for healthcare professionals to effectively use these new tools.
Ethical Considerations
The integration of AI in healthcare raises important ethical considerations. Bias in AI algorithms can lead to disparities in treatment outcomes, potentially exacerbating existing health inequities. Careful consideration must be given to ensuring algorithm fairness and transparency, making sure that AI does not perpetuate or amplify existing societal biases.
Furthermore, questions regarding accountability and responsibility need to be addressed. If an AI system makes a mistake, who is responsible? Developing clear guidelines and protocols for managing such situations is crucial for the responsible implementation of AI in healthcare settings.
Data Security and Privacy
Ensuring the security and privacy of patient data is paramount when integrating AI into treatment protocols. Robust data encryption and access controls are essential to protect sensitive information from unauthorized access or breaches. Strict adherence to data privacy regulations, such as HIPAA in the US, is critical to maintaining patient trust and compliance.
Additionally, transparent data governance policies and procedures should be established to ensure that data is used ethically and responsibly. This includes clear communication with patients about how their data will be used and providing them with control over their information.
Read more about AI for Bipolar Disorder: Managing Mood Swings with Smart Tools
Hot Recommendations
- AI Driven Personalized Sleep Training for Chronic Insomnia
- AI Driven Personalization for Sustainable Stress Management
- Your Personalized Guide to Overcoming Limiting Beliefs
- Understanding Gender Dysphoria and Mental Health Support
- The Power of Advocacy: Mental Health Initiatives Reshaping Society
- Building a Personalized Self Compassion Practice for Self Worth
- The Ethics of AI in Mental Wellness: What You Need to Know
- AI Driven Insights into Your Unique Stress Triggers for Personalized Management
- Beyond Awareness: Actionable Mental Health Initiatives for Lasting Impact
- Creating a Personalized Sleep Hygiene Plan for Shift Workers