AI Driven Personalized Therapies: The Future of Mental Health
Understanding the Need for Personalized Treatment Plans
Modern healthcare increasingly recognizes that standardized treatment protocols often fail to deliver ideal results. The complex interplay between genetic makeup, daily habits, and environmental influences means each patient responds uniquely to medical interventions. Customized care strategies, powered by comprehensive data analysis, aim to address these individual differences by creating targeted approaches for each person's specific requirements. This methodology promotes more successful treatments while reducing unwanted side effects and enhancing overall health improvements.
The Role of Advanced Computing in Custom Care
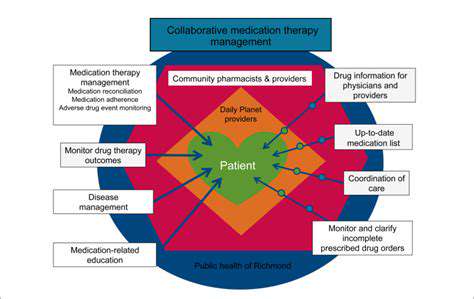
Modern computational systems have become indispensable in developing individualized care strategies. These systems process enormous quantities of patient information, including complete medical backgrounds, DNA profiles, daily routine details, and even geographical data to detect patterns and forecast how individuals might react to various treatments. This depth of analysis empowers medical professionals to make precisely calibrated decisions, choosing therapeutic approaches with the highest probability of effectiveness and safety for each unique case.
Traditional analytical methods frequently struggle with the overwhelming amount and complexity of modern medical data, often resulting in less precise treatment recommendations.
Creating Bespoke Treatment Strategies
Truly personalized healthcare extends far beyond simple dosage adjustments. It encompasses the development of complete, multifaceted intervention plans that might include nutrition programs designed around individual metabolic rates, physical activity regimens optimized for particular health challenges, or medication choices informed by genetic risk factors. The objective is to craft comprehensive solutions that account for all relevant aspects of a patient's unique physiological profile.
Continuous Monitoring and Plan Refinement
Effective individualized care demands ongoing observation and strategy refinement. Modern tracking systems can monitor patient responses continuously, detecting subtle changes in treatment effectiveness. This enables timely modifications to the care plan, maintaining optimal therapeutic impact while minimizing potential complications. The capacity to adapt treatment approaches dynamically as a patient's condition changes represents a crucial benefit of personalized medicine.
Ethical Implications and Evolving Possibilities
While computational systems offer tremendous opportunities for customized care, important ethical questions must be considered. Protecting sensitive health information, ensuring system security, and guaranteeing fair access to these advanced technologies remain critical concerns. The evolution of bespoke medical solutions powered by artificial intelligence presents exciting prospects, but responsible development and ethical implementation are essential to maximize benefits while reducing potential drawbacks. Continued investigation and cooperation between medical practitioners and technology experts will be vital for addressing these challenges and ensuring the principled application of these powerful tools.
AI-Assisted Therapy: Expanding Access and Improving Support

Broadening Mental Health Service Availability
Technology-enhanced therapeutic support represents a groundbreaking opportunity to make mental health services more widely available, particularly in areas with limited access to qualified specialists. These innovations have the power to make psychological support more universally accessible, providing convenient and cost-effective options for those seeking assistance. Remote delivery capabilities are particularly transformative, enabling individuals in isolated locations or with limited mobility to participate in therapeutic sessions without leaving their homes.
The availability of these digital tools can also dramatically reduce waiting periods associated with conventional therapy. Many people experience significant delays before receiving professional help, which can negatively impact their psychological well-being. Digital platforms can streamline initial assessments and matching processes, potentially accelerating the path to appropriate care.
Enhancing Therapeutic Effectiveness
Advanced analytical systems can identify meaningful patterns in patient information, giving therapists valuable insights to customize treatment approaches. This personalized methodology can result in more precisely targeted interventions, specifically designed for each individual's needs and characteristics.
Additionally, these technological tools can provide continuous progress tracking and feedback, allowing therapists to monitor developments and make necessary treatment adjustments. This ongoing evaluation and refinement process is essential for maximizing therapeutic effectiveness and ensuring patients receive the most appropriate support.
By detecting potential risk factors and early warning signs, these systems can help prevent crises and support overall mental wellness. This forward-looking approach can contribute to better treatment results and enhanced life quality for patients.
Ethical Questions and Future Development
While technology-assisted therapy shows great potential, it's essential to carefully consider the ethical implications of its implementation. Protecting patient confidentiality and ensuring data security are paramount concerns that demand robust protective measures. Thoughtful creation and application of ethical standards are necessary to guarantee responsible and trustworthy use of these innovations.
The future of digital therapy will likely involve a cooperative model, combining human therapeutic expertise with advanced analytical capabilities. This integrated approach can create a more comprehensive and effective mental health support system, utilizing the complementary strengths of human insight and technological advancement. Continuous research and refinement will be needed to perfect these tools and ensure they meet changing population needs.
Ongoing assessment of how these digital therapeutic tools affect different population groups is essential to guarantee fair access and outcomes. This constant evaluation is critical for identifying potential biases and ensuring these technologies benefit everyone equally, regardless of background or circumstances.
Beyond Diagnosis: Predictive Analytics for Early Intervention
Fundamentals of Predictive Healthcare Analysis
Advanced predictive methods in healthcare utilize historical patient information combined with sophisticated algorithms to anticipate potential health developments. This methodology enables medical professionals to identify at-risk individuals before symptoms become severe, allowing for proactive care approaches. By examining comprehensive datasets, healthcare providers can uncover subtle patterns that conventional methods might miss, ultimately improving patient outcomes.
Incorporating machine learning into clinical practice allows for continuous updates to risk evaluations as new information becomes available. This dynamic process helps create customized treatment strategies aligned with each patient's distinct health profile. Consequently, predictive analysis not only improves early detection but also optimizes resource utilization within healthcare networks.
Data Gathering for Accurate Predictions
Effective predictive analysis begins with thorough data collection, including electronic medical records, wearable device outputs, genetic profiles, and patient-reported information. High-quality, diverse datasets are fundamental for building reliable models capable of accurate predictions across different populations. Maintaining strict data privacy and regulatory compliance remains a crucial component of this process.
Advanced data collection methods, such as real-time monitoring through connected devices, provide continuous health status updates. This live data enhances predictive models, enabling timely interventions that can halt disease progression. Integrating multiple data sources improves the accuracy of early warning systems, making predictive analytics a potent tool for customized medicine.
Advanced Algorithms in Preventive Care
Sophisticated computational models including decision trees, neural networks, and support vector machines form the foundation of predictive analysis. These systems analyze complex datasets to identify subtle indicators of future health risks. Their ability to learn from new information ensures predictions become increasingly accurate over time, enhancing their clinical value.
Implementing these algorithms requires careful variable selection and model testing to prevent inaccuracies and ensure dependability. When properly applied, machine learning can forecast the onset of chronic conditions like diabetes or heart disease, often years before traditional diagnostic methods. This early detection capability is transformative for preventive medicine.
Customized Preventative Measures
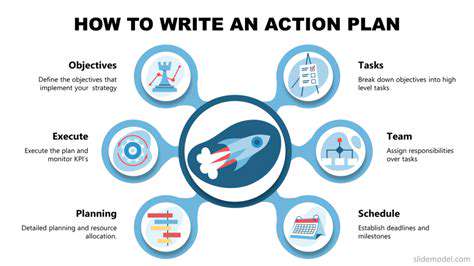
When predictive models identify high-risk individuals, healthcare providers can develop personalized prevention plans tailored to specific needs. These interventions may include lifestyle adjustments, targeted treatments, or increased monitoring frequency. The goal is to prevent disease advancement and enhance quality of life through proactive measures.
Personalization also involves considering economic factors, patient preferences, and behavioral insights to improve engagement and adherence. Technology-supported interventions, such as mobile health applications and remote consultations, facilitate continuous patient involvement outside clinical environments. This integrated approach maximizes the advantages of early prediction and intervention.
Implementation Challenges and Ethical Issues
Despite its potential, predictive analysis faces obstacles related to data quality, model interpretation, and possible biases. Incomplete or inaccurate data can lead to incorrect predictions, potentially damaging patient trust or resulting in unnecessary treatments. Ensuring algorithm transparency and explainability is vital for clinical acceptance.
Ethical considerations also include protecting patient privacy and addressing healthcare access disparities. There's a risk that predictive models might unintentionally reinforce existing inequalities if not carefully designed. Continuous oversight and inclusive data practices are necessary to address these concerns and ensure equitable health outcomes.
The Future of AI in Preventive Healthcare
The integration of AI-powered predictive analysis is set to transform early intervention approaches across healthcare sectors. As models become more advanced, they will enable earlier disease detection, potentially before clinical symptoms appear. This proactive methodology promises to shift healthcare focus from reactive treatment to preventive care.
Advances in wearable technology, genetic research, and data sharing will further enhance customization, allowing interventions to be tailored with unprecedented precision. Collaboration among clinicians, data experts, and policymakers will be crucial in establishing standards and frameworks that maximize benefits while minimizing risks. The future of AI-enhanced early intervention holds tremendous potential for improving global health outcomes.
Ethical Considerations and Future Directions
Moral Implications of AI-Powered Custom Therapies
The incorporation of artificial intelligence into personalized treatments presents numerous ethical challenges that require careful consideration. A primary concern involves protecting sensitive health information. Patient data used to train and refine AI systems must be secured against unauthorized access and misuse. Strong encryption and data anonymization techniques are essential for maintaining patient confidentiality and preserving trust in these systems.
Additionally, ensuring equal access to these advanced therapies is crucial. Differences in economic status and geographic location could create unequal access to the benefits of customized medicine. Developing strategies to bridge these gaps and ensure fair distribution of these innovative treatments is essential for creating an equitable healthcare system.
Algorithmic Fairness and Bias Mitigation
AI systems learn from massive datasets, and if these collections reflect existing societal prejudices, the resulting models may perpetuate or even intensify those biases. This creates significant challenges for maintaining fairness and objectivity in AI-driven personalized treatments. Rigorous testing and validation processes are necessary to identify and correct potential biases in the algorithms, ensuring therapies are applied fairly across diverse populations.
Special attention must be paid to how algorithmic biases might disproportionately affect certain demographic groups. Proactively and transparently addressing these biases is essential to prevent AI-driven treatments from worsening existing health disparities. This requires constant monitoring and evaluation of the algorithms' performance.
Transparency in AI Decision-Making
The opaque nature of some AI models presents challenges in personalized treatment contexts. Both patients and healthcare providers need to understand how the system arrives at its recommendations. Developing AI models that are transparent and explainable is crucial for building trust and accountability. Techniques that explain AI decisions can provide valuable insights into the algorithm's reasoning process, allowing for better understanding and validation of its suggestions.
Responsibility for AI-Generated Recommendations
Determining accountability for decisions made by AI systems in personalized treatments presents significant ethical challenges. Who bears responsibility if an AI system makes an incorrect diagnosis or treatment suggestion? Establishing clear responsibility and accountability protocols is essential for preventing errors and ensuring patient safety. This likely requires multidisciplinary teams including clinicians, AI specialists, and ethicists working together to create comprehensive oversight mechanisms.
Future Development of AI-Enhanced Therapies
The future of AI-driven personalized treatments holds enormous potential, but requires careful consideration of emerging technologies. Ongoing research in areas like deep learning, natural language processing, and sensor technology will likely lead to more sophisticated and personalized treatments. However, maintaining ethical standards in this rapidly evolving field is crucial, including continuous algorithm monitoring for biases, developing robust evaluation methods, and ensuring responsible innovation.
Patient Consent and Data Control
Patient permission is fundamental in AI-assisted personalized treatments. Individuals must be fully informed about how their data will be used, stored, and protected. Clear and understandable consent procedures are essential. Moreover, patients should maintain control over their information, with the ability to access, modify, or delete their data as desired. This necessitates comprehensive data governance frameworks that respect patient autonomy and data ownership rights.
Read more about AI Driven Personalized Therapies: The Future of Mental Health
Hot Recommendations
- AI Driven Personalized Sleep Training for Chronic Insomnia
- AI Driven Personalization for Sustainable Stress Management
- Your Personalized Guide to Overcoming Limiting Beliefs
- Understanding Gender Dysphoria and Mental Health Support
- The Power of Advocacy: Mental Health Initiatives Reshaping Society
- Building a Personalized Self Compassion Practice for Self Worth
- The Ethics of AI in Mental Wellness: What You Need to Know
- AI Driven Insights into Your Unique Stress Triggers for Personalized Management
- Beyond Awareness: Actionable Mental Health Initiatives for Lasting Impact
- Creating a Personalized Sleep Hygiene Plan for Shift Workers